Introduction
Researchers from the Critical Analytics for Manufacturing Personalized Medicine (CAMP) interdisciplinary research group at the Singapore-MIT Alliance for Research and Technology (SMART), MIT’s research enterprise in Singapore, along with collaborators from the National University of Singapore’s Tissue Engineering Program, have developed a novel method to enhance the ability of mesenchymal stromal cells (MSCs) to generate cartilage tissue by adding ascorbic acid during MSC expansion. The study also found that micro-magnetic resonance relaxometry (µMRR), a new process analytical tool developed by SMART CAMP, can be used as a rapid, label-free process monitoring tool for MSC quality expansion.
Background
Articular cartilage, a connective tissue that protects the ends of bones in joints, can deteriorate due to injury, aging, or arthritis, leading to significant joint pain and disability. This is particularly concerning in countries like Singapore, which have an active and aging population, as articular cartilage degeneration is a growing condition affecting more people. Autologous chondrocyte implantation is currently the only FDA-approved cell therapy for articular cartilage injuries, but it is expensive, time-consuming, and requires multiple treatments. MSCs offer a promising alternative due to their good safety profiles for transplantation. However, clinical use of MSCs is limited due to inconsistent treatment outcomes caused by factors such as donor-to-donor variability, cell variation during expansion, and non-standardized MSC manufacturing protocols.
Challenges and Solutions
MSCs’ heterogeneity can lead to variations in their biological behavior and treatment outcomes. While large-scale MSC expansions are necessary to obtain a therapeutically relevant number of cells for implantation, this process can introduce cellular heterogeneity. Therefore, improved processes are essential to reduce cellular heterogeneity while increasing donor cell numbers with enhanced chondrogenic potential—the ability of MSCs to differentiate into cartilage cells to repair cartilage tissue—paving the way for more effective and consistent MSC-based therapies.
Research Findings
In a paper titled « Metabolic Modulation to Enhance MSC Expansion and Therapeutic Potential for Articular Cartilage Repair« , published in the scientific journal Stem Cell Research & Therapy, CAMP researchers detailed their development of a priming strategy to improve MSC quality expansion by altering how cells use energy. The research results showed a positive correlation between chondrogenic potential and oxidative phosphorylation (OXPHOS), a process that exploits oxygen reduction to create adenosine triphosphate, an energy source driving and supporting many processes in living cells. This suggests that manipulating MSC metabolism is a promising strategy to enhance chondrogenic potential.
Methodology
Using new PATs developed by CAMP, researchers explored the potential of metabolic modulation in short- and long-term cell harvesting and reseeding. To enhance their chondrogenic potential, they varied the nutritional composition, including glucose, pyruvate, glutamine, and ascorbic acid (AA). As AA is reported to support OXPHOS and its positive impact on chondrogenic potential during differentiation—a process where immature cells become mature cells with specific functions—researchers further investigated its effects during MSC expansion.
Results
Adding AA to cell cultures for one passage during MSC expansion and before differentiation onset improved chondrogenic differentiation, a critical quality attribute (CQA) for better articular cartilage repair. Longer-term AA treatment led to over a 300-fold increase in MSC yield with enhanced chondrogenic potential, along with reduced cellular heterogeneity and senescence—a process where a cell ages and permanently stops dividing but does not die—compared to untreated cells. AA-treated MSCs with improved chondrogenic potential showed a significant metabolic profile shift towards OXPHOS. This metabolic shift correlated with µMRR measurements, identifying new CQAs that could be implemented in MSC manufacturing for articular cartilage repair.
Conclusion
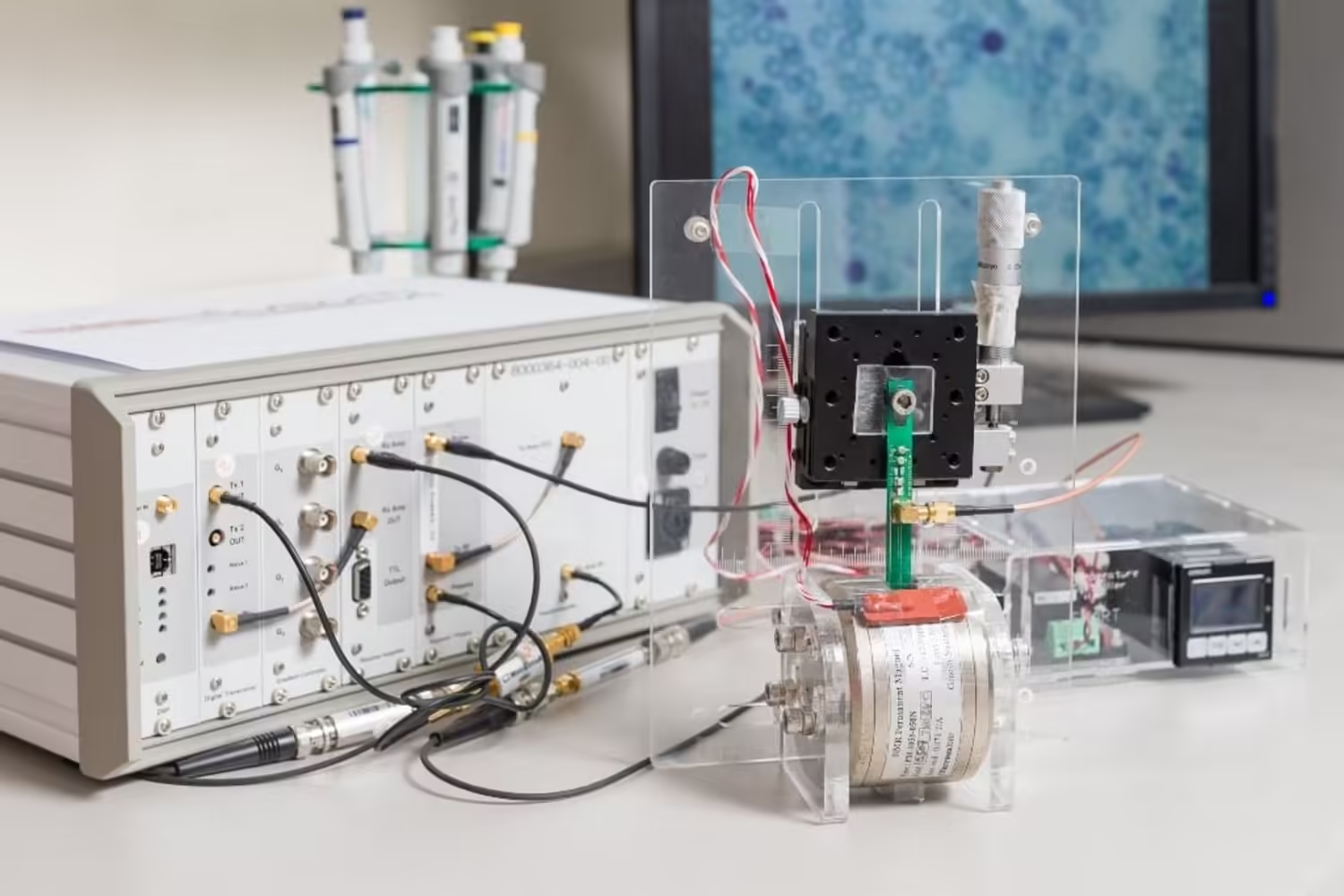
The research also demonstrates the potential of the process analytical tool developed by CAMP, micro-magnetic resonance relaxometry (µMRR)—a miniature benchtop device using magnetic resonance imaging (MRI) at a microscopic scale—as a process monitoring tool for MSC expansion with AA supplementation. Initially used as a label-free malaria diagnostic method due to the presence of paramagnetic hemozoin particles, µMRR was used in the research to detect MSC senescence. This rapid, label-free method requires only a small number of cells for evaluation, allowing MSC therapy manufacturing in closed systems—a system protecting pharmaceutical products by reducing contamination risks from the external environment—while enabling intermittent monitoring of a limited batch size by production.
« Donor-to-donor variation, intrapopulation heterogeneity, and cellular senescence have hindered MSC success as a standard treatment for articular cartilage repair. Our research has shown that AA supplementation during MSC expansion can overcome these bottlenecks and enhance MSC chondrogenic potential, » explains Ching Ann Tee, senior postdoctoral associate at SMART CAMP and first author of the paper. « By controlling metabolic conditions such as AA supplementation, coupled with CAMP’s process analytical tools like µMRR, cell therapy product yield and quality could be significantly increased. This major advancement could help make MSC therapy a more effective and viable treatment option and provide standards to improve the manufacturing pipeline. »
« This approach of using metabolic modulation to enhance MSC chondrogenic potential could be adapted to similar concepts for other therapeutic indications, such as osteogenic potential for bone repair or other types of stem cells. Implementing our findings in MSC manufacturing settings could be a significant advancement for patients suffering from osteoarthritis and other joint diseases, as we can efficiently produce large quantities of high-quality MSCs with consistent functionality and enable treatment for more patients, » adds Professor Laurie A. Boyer, principal investigator at SMART CAMP, professor of biology and biological engineering at MIT, and corresponding author of the paper.
The research is conducted by SMART and supported by the National Research Foundation Singapore under its Campus for Research Excellence and Technological Enterprise program.